Page 92 - Remedial Andrology
P. 92
of the disease [994, 995]. Palpable plaques have been reported as an initial symptom in 39% of the patients
and mostly situated dorsally [50, 997].
In addition to functional effects on sexual intercourse, men may also suffer from significant psychological
distress. Validated mental health questionnaires have shown that 48% of men with PD have moderate or
severe depression, sufficient to warrant medical evaluation [998].
8.2.1.5 Summary of evidence on epidemiology/aetiology/pathophysiology of Peyronie’s disease
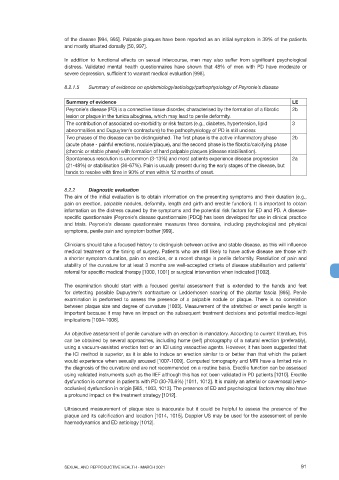
Summary of evidence LE
Peyronie’s disease (PD) is a connective tissue disorder, characterised by the formation of a fibrotic 2b
lesion or plaque in the tunica albuginea, which may lead to penile deformity.
The contribution of associated co-morbidity or risk factors (e.g., diabetes, hypertension, lipid 3
abnormalities and Dupuytren’s contracture) to the pathophysiology of PD is still unclear.
Two phases of the disease can be distinguished. The first phase is the active inflammatory phase 2b
(acute phase - painful erections, nodule/plaque), and the second phase is the fibrotic/calcifying phase
(chronic or stable phase) with formation of hard palpable plaques (disease stabilisation).
Spontaneous resolution is uncommon (3-13%) and most patients experience disease progression 2a
(21-48%) or stabilisation (36-67%). Pain is usually present during the early stages of the disease, but
tends to resolve with time in 90% of men within 12 months of onset.
8.2.2 Diagnostic evaluation
The aim of the initial evaluation is to obtain information on the presenting symptoms and their duration (e.g.,
pain on erection, palpable nodules, deformity, length and girth and erectile function). It is important to obtain
information on the distress caused by the symptoms and the potential risk factors for ED and PD. A disease-
specific questionnaire (Peyronie’s disease questionnaire [PDQ]) has been developed for use in clinical practice
and trials. Peyronie’s disease questionnaire measures three domains, including psychological and physical
symptoms, penile pain and symptom bother [999].
Clinicians should take a focused history to distinguish between active and stable disease, as this will influence
medical treatment or the timing of surgery. Patients who are still likely to have active disease are those with
a shorter symptom duration, pain on erection, or a recent change in penile deformity. Resolution of pain and
stability of the curvature for at least 3 months are well-accepted criteria of disease stabilisation and patients’
referral for specific medical therapy [1000, 1001] or surgical intervention when indicated [1002].
The examination should start with a focused genital assessment that is extended to the hands and feet
for detecting possible Dupuytren’s contracture or Ledderhosen scarring of the plantar fascia [995]. Penile
examination is performed to assess the presence of a palpable nodule or plaque. There is no correlation
between plaque size and degree of curvature [1003]. Measurement of the stretched or erect penile length is
important because it may have an impact on the subsequent treatment decisions and potential medico-legal
implications [1004-1006].
An objective assessment of penile curvature with an erection is mandatory. According to current literature, this
can be obtained by several approaches, including home (self) photography of a natural erection (preferably),
using a vacuum-assisted erection test or an ICI using vasoactive agents. However, it has been suggested that
the ICI method is superior, as it is able to induce an erection similar to or better than that which the patient
would experience when sexually aroused [1007-1009]. Computed tomography and MRI have a limited role in
the diagnosis of the curvature and are not recommended on a routine basis. Erectile function can be assessed
using validated instruments such as the IIEF although this has not been validated in PD patients [1010]. Erectile
dysfunction is common in patients with PD (30-70.6%) [1011, 1012]. It is mainly an arterial or cavernosal (veno-
occlusive) dysfunction in origin [985, 1003, 1013]. The presence of ED and psychological factors may also have
a profound impact on the treatment strategy [1012].
Ultrasound measurement of plaque size is inaccurate but it could be helpful to assess the presence of the
plaque and its calcification and location [1014, 1015]. Doppler US may be used for the assessment of penile
haemodynamics and ED aetiology [1012].
SEXUAL AND REPRODUCTIVE HEALTH - MARCH 2021 91