Page 83 - Remedial Andrology
P. 83
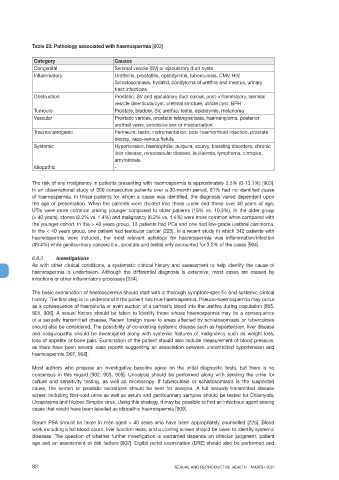
Table 23: Pathology associated with haemospermia [902]
Category Causes
Congenital Seminal vesicle (SV) or ejaculatory duct cysts
Inflammatory Urethritis, prostatitis, epididymitis, tuberculosis, CMV, HIV,
Schistosomiasis, hydatid, condyloma of urethra and meatus, urinary
tract infections
Obstruction Prostatic, SV and ejaculatory duct calculi, post-inflammatory, seminal
vesicle diverticula/cyst, urethral stricture, utricle cyst, BPH
Tumours Prostate, bladder, SV, urethra, testis, epididymis, melanoma
Vascular Prostatic varices, prostatic telangiectasia, haemangioma, posterior
urethral veins, excessive sex or masturbation
Trauma/iatrogenic Perineum, testis, instrumentation, post-haemorrhoid injection, prostate
biopsy, vaso-venous fistula
Systemic Hypertension, haemophilia, purpura, scurvy, bleeding disorders, chronic
liver disease, renovascular disease, leukaemia, lymphoma, cirrhosis,
amyloidosis
Idiopathic -
The risk of any malignancy in patients presenting with haemospermia is approximately 3.5% (0-13.1%) [903].
In an observational study of 300 consecutive patients over a 30-month period, 81% had no identified cause
of haemospermia. In those patients for whom a cause was identified, the diagnosis varied dependent upon
the age of presentation. When the patients were divided into those under and those over 40 years of age,
UTIs were more common among younger compared to older patients (15% vs. 10.3%). In the older group
(> 40 years), stones (2.2% vs. 1.4%) and malignancy (6.2% vs. 1.4%) were more common when compared with
the younger cohort. In the > 40 years group, 13 patients had PCa and one had low-grade urethral carcinoma.
In the < 40 years group, one patient had testicular cancer [223]. In a recent study in which 342 patients with
haemospermia were included, the most relevant aetiology for haemospermia was inflammation/infection
(49.4%) while genitourinary cancers (i.e., prostate and testis) only accounted for 3.2% of the cases [904].
6.8.3 Investigations
As with other clinical conditions, a systematic clinical history and assessment to help identify the cause of
haemospermia is undertaken. Although the differential diagnosis is extensive, most cases are caused by
infections or other inflammatory processes [224].
The basic examination of haemospermia should start with a thorough symptom-specific and systemic clinical
history. The first step is to understand if the patient has true haemospermia. Pseudo-haemospermia may occur
as a consequence of haematuria or even suction of a partner’s blood into the urethra during copulation [865,
905, 906]. A sexual history should be taken to identify those whose haemospermia may be a consequence
of a sexually transmitted disease. Recent foreign travel to areas affected by schistosomiasis or tuberculosis
should also be considered. The possibility of co-existing systemic disease such as hypertension, liver disease
and coagulopathy should be investigated along with systemic features of malignancy such as weight loss,
loss of appetite or bone pain. Examination of the patient should also include measurement of blood pressure,
as there have been several case reports suggesting an association between uncontrolled hypertension and
haemospermia [907, 908].
Most authors who propose an investigative baseline agree on the initial diagnostic tests, but there is no
consensus in this regard [902, 903, 905]. Urinalysis should be performed along with sending the urine for
culture and sensitivity testing, as well as microscopy. If tuberculosis or schistosomiasis is the suspected
cause, the semen or prostatic secretions should be sent for analysis. A full sexually-transmitted disease
screen including first-void urine as well as serum and genitourinary samples should be tested for Chlamydia,
Ureaplasma and Herpes Simplex virus. Using this strategy, it may be possible to find an infectious agent among
cases that would have been labelled as idiopathic haemospermia [909].
Serum PSA should be taken in men aged > 40 years who have been appropriately counselled [225]. Blood
work including a full blood count, liver function tests, and a clotting screen should be taken to identify systemic
diseases. The question of whether further investigation is warranted depends on clinician judgment, patient
age and an assessment of risk factors [902]. Digital rectal examination (DRE) should also be performed and
82 SEXUAL AND REPRODUCTIVE HEALTH - MARCH 2021