Page 128 - Remedial Andrology
P. 128
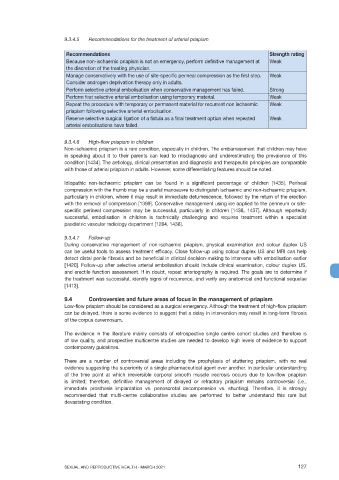
9.3.4.5 Recommendations for the treatment of arterial priapism
Recommendations Strength rating
Because non-ischaemic priapism is not an emergency, perform definitive management at Weak
the discretion of the treating physician.
Manage conservatively with the use of site-specific perineal compression as the first step. Weak
Consider androgen deprivation therapy only in adults.
Perform selective arterial embolisation when conservative management has failed. Strong
Perform first selective arterial embolisation using temporary material. Weak
Repeat the procedure with temporary or permanent material for recurrent non ischaemic Weak
priapism following selective arterial embolisation.
Reserve selective surgical ligation of a fistula as a final treatment option when repeated Weak
arterial embolisations have failed.
9.3.4.6 High-flow priapism in children
Non-ischaemic priapism is a rare condition, especially in children. The embarrassment that children may have
in speaking about it to their parents can lead to misdiagnosis and underestimating the prevalence of this
condition [1434]. The aetiology, clinical presentation and diagnostic and therapeutic principles are comparable
with those of arterial priapism in adults. However, some differentiating features should be noted.
Idiopathic non-ischaemic priapism can be found in a significant percentage of children [1435]. Perineal
compression with the thumb may be a useful manoeuvre to distinguish ischaemic and non-ischaemic priapism,
particularly in children, where it may result in immediate detumescence, followed by the return of the erection
with the removal of compression [1399]. Conservative management using ice applied to the perineum or site-
specific perineal compression may be successful, particularly in children [1436, 1437]. Although reportedly
successful, embolisation in children is technically challenging and requires treatment within a specialist
paediatric vascular radiology department [1284, 1438].
9.3.4.7 Follow-up
During conservative management of non-ischaemic priapism, physical examination and colour duplex US
can be useful tools to assess treatment efficacy. Close follow-up using colour duplex US and MRI can help
detect distal penile fibrosis and be beneficial in clinical decision-making to intervene with embolisation earlier
[1420]. Follow-up after selective arterial embolisation should include clinical examination, colour duplex US,
and erectile function assessment. If in doubt, repeat arteriography is required. The goals are to determine if
the treatment was successful, identify signs of recurrence, and verify any anatomical and functional sequelae
[1413].
9.4 Controversies and future areas of focus in the management of priapism
Low-flow priapism should be considered as a surgical emergency. Although the treatment of high-flow priapism
can be delayed, there is some evidence to suggest that a delay in intervention may result in long-term fibrosis
of the corpus cavernosum.
The evidence in the literature mainly consists of retrospective single centre cohort studies and therefore is
of low quality, and prospective multicentre studies are needed to develop high levels of evidence to support
contemporary guidelines.
There are a number of controversial areas including the prophylaxis of stuttering priapism, with no real
evidence suggesting the superiority of a single pharmaceutical agent over another. In particular understanding
of the time point at which irreversible corporal smooth muscle necrosis occurs due to low-flow priapism
is limited; therefore, definitive management of delayed or refractory priapism remains controversial (i.e.,
immediate prosthesis implantation vs. penoscrotal decompression vs. shunting). Therefore, it is strongly
recommended that multi-centre collaborative studies are performed to better understand this rare but
devastating condition.
SEXUAL AND REPRODUCTIVE HEALTH - MARCH 2021 127