Page 125 - Remedial Andrology
P. 125
study revealed that 90% of men with SCD had their first priapism episode before age 20 years [1353]. Priapism
in children should be evaluated and treated in a timely manner, as untreated ischaemic priapism may lead to
ED and psychosexual disorders in adulthood [1393]. A multi-disciplinary team approach should be utilised with
specialist input from haematologists and paediatric endocrinologists.
9.3 Non-ischaemic (high-flow or arterial) priapism
Most of the identified studies were small retrospective case series reporting principally on the role of
embolisation in post-traumatic non-ischaemic priapism (Appendix 5). This may reflect the uncommon nature
of the condition. Success rates and erectile function were well documented across all reports. Some studies
attempted to stratify outcomes based on the agent used for embolisation (e.g., microcoil or autologous clot),
although care should be taken when interpreting case series with small patient numbers.
9.3.1 Epidemiology/aetiology/pathophysiology
Epidemiological data on non-ischaemic priapism are almost exclusively derived from small case series [1243,
1274, 1276, 1394, 1395]. Non-ischaemic priapism is significantly less common than the ischaemic type,
comprising only 5% of all priapism cases [1243]. The most frequent cause of non-ischaemic priapism is blunt
perineal or penile trauma [1396]. The injury results in a laceration in the cavernosal artery or branches, leading
to a fistula between the artery and the lacunar spaces of the sinusoidal space [1395]. The resultant increased
blood flow results in a persistent and prolonged erection [1397].
There is often a delay between the trauma and the development of the priapism that may be up to two to
three weeks [1398]. This is suggested to reflect either spasm or ischaemic necrosis of the injured artery, with
the fistula only developing as the spasm resolves or when the ischaemic segment “blows up”. The priapism
typically occurs after a nocturnal erection or an erection related to sexual activity, resulting in the sudden
increase of blood flow and pressure in the cavernous arteries [1399]. The patient typically reports an erection
that is not fully rigid and is not associated with pain because the venous drainage is not compromised and the
penile tissue does not become ischaemic [1400].
Non-ischaemic priapism can occur after acute spinal cord injury, presumably due to loss of sympathetic input,
leading to predominant parasympathetic input and increased arterial flow [1401]. It has also been reported to
occur following internal urethrotomy [1402], Nesbit procedure [1403], circumcision [1404], transrectal prostate
biopsy [1405], and brachytherapy for prostate cancer [1406]. Some cases have also been described following
shunting procedures performed for ischaemic priapism due to a lacerated cavernosal artery (conversion of
low-flow to high-flow priapism) [1407-1409]. Although SCD is usually associated with ischaemic priapism,
occasional cases of high-flow priapism have been reported; however, the pathophysiological mechanism
remains unclear [1410]. Finally, metastatic malignancy to the penis can also rarely cause non-ischaemic
priapism [1411, 1412] (Table 38).
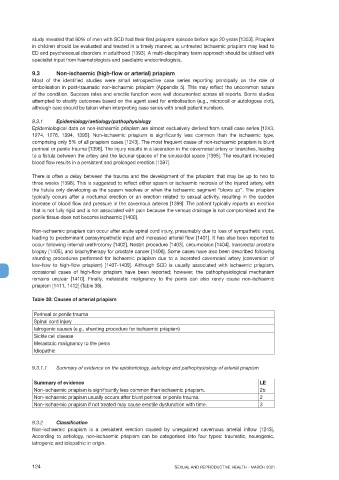
Table 38: Causes of arterial priapism
Perineal or penile trauma
Spinal cord injury
Iatrogenic causes (e.g., shunting procedure for ischaemic priapism)
Sickle cell disease
Metastatic malignancy to the penis
Idiopathic
9.3.1.1 Summary of evidence on the epidemiology, aetiology and pathophysiology of arterial priapism
Summary of evidence LE
Non-ischaemic priapism is significantly less common than ischaemic priapism. 2b
Non-ischaemic priapism usually occurs after blunt perineal or penile trauma. 2
Non-ischaemic priapism if not treated may cause erectile dysfunction with time. 3
9.3.2 Classification
Non-ischaemic priapism is a persistent erection caused by unregulated cavernous arterial inflow [1243].
According to aetiology, non-ischaemic priapism can be categorised into four types: traumatic, neurogenic,
iatrogenic and idiopathic in origin.
124 SEXUAL AND REPRODUCTIVE HEALTH - MARCH 2021