Page 126 - Remedial Andrology
P. 126
9.3.3 Diagnostic evaluation
9.3.3.1 History
A comprehensive history is mandatory in non-ischaemic priapism diagnosis and follows the same principles
as described in Table 33. Arterial priapism should be suspected when the patient reports a history of pelvic,
perineal, or genital trauma; no penile pain (discomfort is possible); and a persistent, not fully rigid erection
(Table 34). The corpus cavernosum can become fully rigid with sexual stimulation, so the sexual intercourse
is usually not compromised. The onset of post-traumatic non-ischaemic priapism can be delayed by several
hours to weeks following the initial injury [1243].
9.3.3.2 Physical examination
In non-ischaemic priapism, the corpora are tumescent but not fully rigid. Abdominal, penile and perineal
examination may reveal evidence of trauma (Table 34) [1243]. Neurological examination is indicated if a
neurogenic aetiology is suspected.
9.3.3.3 Laboratory testing
Laboratory testing should include a blood count with white blood cell differential and a coagulation profile to
assess for anaemia and other haematological abnormalities. Blood aspiration from the corpus cavernosum
shows bright red arterial blood in arterial priapism, while blood is dark in ischaemic priapism (Table 34) (LE:
2b). Blood gas analysis is essential to differentiate between non-ischaemic and ischaemic priapism. Blood gas
values in high-flow priapism show normal arterial blood [1243] (Table 35).
9.3.3.4 Penile imaging
Colour duplex US of the penis and perineum is recommended and can differentiate non-ischaemic from
ischaemic priapism [1272-1274]. Ultrasound must be performed without intracavernosal vasoactive drug
injection [1413]. In non-ischaemic priapism, US helps to localise the fistula site and appears as a characteristic
colour blush and turbulent high-velocity flow on Doppler analysis [1414]. Patients with non-ischaemic priapism
have normal to high blood velocities in the cavernous arteries [1245, 1415].
Selective pudendal arteriography can reveal a characteristic blush at the site of injury in arterial priapism [1416,
1417]. However, due to its invasiveness, it should be reserved for the management of non-ischaemic priapism
when embolisation is being considered [1243, 1268].
The role of MRI in the diagnostic evaluation of priapism is controversial. Its role in non-ischaemic priapism is
limited because the small penile vessels and fistulae cannot be easily demonstrated [1418].
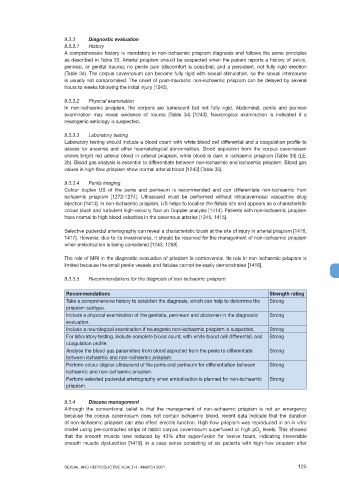
9.3.3.5 Recommendations for the diagnosis of non-ischaemic priapism
Recommendations Strength rating
Take a comprehensive history to establish the diagnosis, which can help to determine the Strong
priapism subtype.
Include a physical examination of the genitalia, perineum and abdomen in the diagnostic Strong
evaluation.
Include a neurological examination if neurogenic non-ischaemic priapism is suspected. Strong
For laboratory testing, include complete blood count, with white blood cell differential, and Strong
coagulation profile.
Analyse the blood gas parameters from blood aspirated from the penis to differentiate Strong
between ischaemic and non-ischaemic priapism.
Perform colour duplex ultrasound of the penis and perineum for differentiation between Strong
ischaemic and non-ischaemic priapism.
Perform selected pudendal arteriography when embolisation is planned for non-ischaemic Strong
priapism.
9.3.4 Disease management
Although the conventional belief is that the management of non-ischaemic priapism is not an emergency
because the corpus cavernosum does not contain ischaemic blood, recent data indicate that the duration
of non-ischaemic priapism can also effect erectile function. High-flow priapism was reproduced in an in vitro
model using pre-contracted strips of rabbit corpus cavernosum superfused at high pO levels. This showed
2
that the smooth muscle tone reduced by 43% after super-fusion for twelve hours, indicating irreversible
smooth muscle dysfunction [1419]. In a case series consisting of six patients with high-flow priapism after
SEXUAL AND REPRODUCTIVE HEALTH - MARCH 2021 125