Page 131 - Remedial Andrology
P. 131
10.3.1.2 Physical examination
Focused physical examination is compulsory in the evaluation of every infertile male, including presence
of secondary sexual characteristics. The size, texture and consistency of the testes must be evaluated. In
clinical practice, testicular volume is assessed by Prader’s orchidometer [1457]; orchidometry may over-
estimate testicular volume when compared with US assessment [1458]. There are no uniform reference values
in terms of Prader’s orchidometer-derived testicular volume, due to differences in the populations studied
(e.g., geographic area, nourishment, ethnicity and environmental factors) [1457-1459]. The mean Prader’s
orchidometer-derived testis volume reported in the European general population is 20.0 ± 5.0 mL [1457],
whereas in infertile patients it is 18.0 ± 5.0 mL [1457, 1460, 1461]. The presence of the vas deferens, fullness of
epididymis and presence of a varicocele should be always determined. Likewise, palpable abnormalities of the
testis, epididymis, and vas deferens should be evaluated. Other physical alterations, such as abnormalities of
the penis (e.g., phimosis, short frenulum, fibrotic nodules, epispadias, hypospadias, etc.), abnormal body hair
distribution and gynecomastia, should also be evaluated.
Typical findings from the physical examination of a patient with characteristics suggestive for testicular
deficiency include:
• abnormal secondary sexual characteristics;
• abnormal testicular volume and/or consistency;
• testicular masses (potentially suggestive of cancer);
• absence of testes (uni-bilaterally);
• gynaecomastia;
• varicocele.
10.3.2 Semen analysis
A comprehensive andrological examination is always indicated in every infertile couple. Important treatment
decisions are based on the results of semen analysis and most studies evaluate semen parameters as
a surrogate outcome for male fertility. However, semen analysis cannot precisely distinguish fertile from
infertile men [1462]; therefore, it is essential that the complete laboratory work-up is standardised according
to reference values (Table 40). Ejaculate analysis has been standardised by the WHO and disseminated by
publication of the most updated version of the WHO Laboratory Manual for the Examination and Processing of
th
Human Semen (5 edn) [1463]. There is consensus that modern semen analysis must follow these guidelines.
However, it has also become clear from studies that more complex testing than semen analysis may be
required, particularly in men belonging to couples with recurrent pregnancy loss from natural conception or
ART and men with unexplained male infertility. Although definitive conclusions cannot be drawn, also given
the heterogeneity of the studies, in these patients there is evidence that sperm DNA may be damaged, thus
resulting in pregnancy failure [1443, 1464, 1465] (see below).
th
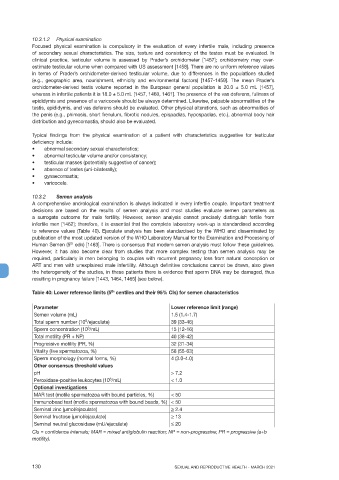
Table 40: Lower reference limits (5 centiles and their 95% CIs) for semen characteristics
Parameter Lower reference limit (range)
Semen volume (mL) 1.5 (1.4-1.7)
Total sperm number (10 /ejaculate) 39 (33-46)
6
6
Sperm concentration (10 /mL) 15 (12-16)
Total motility (PR + NP) 40 (38-42)
Progressive motility (PR, %) 32 (31-34)
Vitality (live spermatozoa, %) 58 (55-63)
Sperm morphology (normal forms, %) 4 (3.0-4.0)
Other consensus threshold values
pH > 7.2
6
Peroxidase-positive leukocytes (10 /mL) < 1.0
Optional investigations
MAR test (motile spermatozoa with bound particles, %) < 50
Immunobead test (motile spermatozoa with bound beads, %) < 50
Seminal zinc (μmol/ejaculate) > 2.4
Seminal fructose (μmol/ejaculate) > 13
Seminal neutral glucosidase (mU/ejaculate) < 20
CIs = confidence intervals; MAR = mixed antiglobulin reaction; NP = non-progressive; PR = progressive (a+b
motility).
130 SEXUAL AND REPRODUCTIVE HEALTH - MARCH 2021