Page 45 - Remedial Andrology
P. 45
[302, 314, 315]. Atrial fibrillation [316], hyperthyroidism [20], vitamin D deficiency [317, 318], hyperuricemia
[319], depression [320], chronic kidney disease [313], rheumatic disease [321] and chronic obstructive
pulmonary disease [322] have also been reported as risks factors. Available data do not confirm a clear
association between ED and hypothyroidism and hyperprolactinaemia [20].
Further epidemiological data have also highlighted other potential risk factors associated with ED
including sleep disorders [323], obstructive sleep apnoea [324], psoriasis [325-327], gouty arthritis [328] and
ankylosing spondylitis [329], non-alcoholic fatty liver disease [330], other chronic liver disorders [331], chronic
periodontitis [332], open-angle glaucoma [333], inflammatory bowel disease [334], chronic fatigue syndrome
[335] and allergic rhinitis [336]. Insufficient data are currently available to correlate primarily organic or primarily
psychogenic ED with SARS-CoV-2 infection associated disease (COVID-19) [337, 338].
Erectile dysfunction is also frequently associated with other urological conditions and procedures (Table 9).
Epidemiological studies have demonstrated consistent evidence for an association between LUTS/BPH and
sexual dysfunction, regardless of age, other co-morbidity and lifestyle factors [339]. The Multinational Survey
on the Aging Male study, performed in the USA, France, Germany, Italy, Netherlands, Spain, and the UK,
systematically investigated the relationship between LUTS and sexual dysfunction in > 12,000 men aged
50-80 years. In the 83% of men who were reported to be sexually active, the overall prevalence of LUTS
was 90%, with an overall 49% prevalence of ED and a reported complete absence of erections in 10% of
patients. The overall prevalence of ejaculatory disorders was 46% [247]. Regardless of the technique used,
surgery for BPH-LUTS had no significant impact on erectile function. A post-operative improvement of erectile
function was even found depending on the degree of LUTS improvement [340, 341]. An association has been
confirmed between ED and CP/CPPS [342], and bladder pain syndrome/interstitial cystitis (BPS/IC), mostly in
younger men [343]. An association between ED and PE has also been demonstrated (see Section 6.2) [344]. An
increased risk of ED is reported following transrectal ultrasound (TRUS)-guided prostate biopsy [345] and after
open urethroplasty, especially for correction of posterior strictures [346], with recent findings emphasising the
importance of patient-reported outcome measures (PROMs) in urethral reconstructive surgery to better report
actual sexual function outcomes [347, 348].
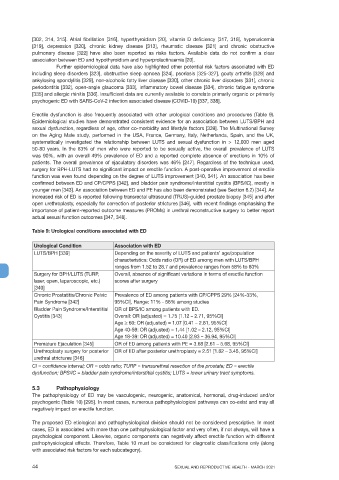
Table 9: Urological conditions associated with ED
Urological Condition Association with ED
LUTS/BPH [339] Depending on the severity of LUTS and patients’ age/population
characteristics: Odds ratio (OR) of ED among men with LUTS/BPH
ranges from 1.52 to 28.7 and prevalence ranges from 58% to 80%
Surgery for BPH/LUTS (TURP, Overall, absence of significant variations in terms of erectile function
laser, open, laparoscopic, etc.) scores after surgery
[340]
Chronic Prostatitis/Chronic Pelvic Prevalence of ED among patients with CP/CPPS 29% [24%-33%,
Pain Syndrome [342] 95%CI], Range: 11% - 56% among studies
Bladder Pain Syndrome/Interstitial OR of BPS/IC among patients with ED.
Cystitis [343] Overall: OR (adjusted) = 1.75 [1.12 – 2.71, 95%CI]
Age > 60: OR (adjusted) = 1.07 [0.41 – 2.81, 95%CI]
Age 40-59: OR (adjusted) = 1.44 [1.02 – 2.12, 95%CI]
Age 18-39: OR (adjusted) = 10.40 [2.93 – 36.94, 95%CI]
Premature Ejaculation [345] OR of ED among patients with PE = 3.68 [2.61 – 5.68, 95%CI]
Urethroplasty surgery for posterior OR of ED after posterior urethroplasty = 2.51 [1.82 – 3.45, 95%CI]
urethral strictures [346]
CI = confidence interval; OR = odds ratio; TURP = transurethral resection of the prostate; ED = erectile
dysfunction; BPS/IC = bladder pain syndrome/interstitial cystitis; LUTS = lower urinary tract symptoms.
5.3 Pathophysiology
The pathophysiology of ED may be vasculogenic, neurogenic, anatomical, hormonal, drug-induced and/or
psychogenic (Table 10) [295]. In most cases, numerous pathophysiological pathways can co-exist and may all
negatively impact on erectile function.
The proposed ED etiological and pathophysiological division should not be considered prescriptive. In most
cases, ED is associated with more than one pathophysiological factor and very often, if not always, will have a
psychological component. Likewise, organic components can negatively affect erectile function with different
pathophysiological effects. Therefore, Table 10 must be considered for diagnostic classifications only (along
with associated risk factors for each subcategory).
44 SEXUAL AND REPRODUCTIVE HEALTH - MARCH 2021