Page 102 - Remedial Andrology
P. 102
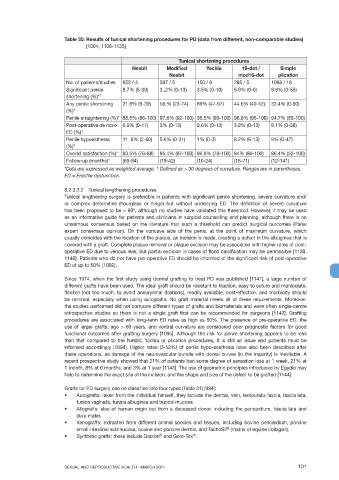
Table 30: Results of tunical shortening procedures for PD (data from different, non-comparable studies)
[1004, 1108-1135]
Tunical shortening procedures
Nesbit Modified Yachia 16-dot / Simple
Nesbit mod16-dot plication
No. of patients/studies 652 / 4 387 / 5 150 / 6 285 / 5 1068 / 18
Significant penile 8.7% (5-39) 3.,2% (0-13) 3.5% (0-10) 5.9% (0-6) 8.9% (0-55)
shortening (%)* †
Any penile shortening 21.8% (9-39) 58.% (23-74) 69% (47-97) 44.6% (40-52). 33.4% (0-90)
(%)*
Penile straightening (%)* 88.5% (86-100) 97.6% (92-100) 95.5% (93-100) 96.9% (95-100) 94.7% (85-100)
Post-operative de novo 6.9% (0-17) 3% (0-13) 9.6% (0-13) 3.8% (0-13) 8.1% (0-38)
ED (%)*
Penile hypoesthesia 11. 8% (2-60) 5.6% (0-31) 1% (0-3) 8.2% (6-13) 9% (0-47)
(%)*
Overall satisfaction (%)* 83.5% (76-88) 95.4% (87-100) 86.8% (78-100) 94% (86-100) 86.4% (52-100)
Follow-up (months)* (69-84) (19-42) (10-24) (18-71) (12-141)
†
*Data are expressed as weighted average. Defined as > 30 degrees of curvature. Ranges are in parentheses.
ED = Erectile dysfunction.
8.2.3.2.2 Tunical lengthening procedures
Tunical lengthening surgery is preferable in patients with significant penile shortening, severe curvature and/
or complex deformities (hourglass or hinge) but without underlying ED. The definition of severe curvature
has been proposed to be > 60 , although no studies have validated this threshold. However, it may be used
o
as an informative guide for patients and clinicians in surgical counselling and planning, although there is no
unanimous consensus based on the literature that such a threshold can predict surgical outcomes (Panel
expert consensus opinion). On the concave side of the penis, at the point of maximum curvature, which
usually coincides with the location of the plaque, an incision is made, creating a defect in the albuginea that is
covered with a graft. Complete plaque removal or plaque excision may be associated with higher rates of post-
operative ED due to venous leak, but partial excision in cases of florid calcification may be permissible [1139,
1140]. Patients who do not have pre-operative ED should be informed of the significant risk of post-operative
ED of up to 50% [1092].
Since 1974, when the first study using dermal grafting to treat PD was published [1141], a large number of
different grafts have been used. The ideal graft should be resistant to traction, easy to suture and manipulate,
flexible (not too much, to avoid aneurysmal dilations), readily available, cost-effective, and morbidity should
be minimal, especially when using autografts. No graft material meets all of these requirements. Moreover,
the studies performed did not compare different types of grafts and biomaterials and were often single-centre
retrospective studies so there is not a single graft that can be recommended for surgeons [1142]. Grafting
procedures are associated with long-term ED rates as high as 50%. The presence of pre-operative ED, the
use of larger grafts, age > 60 years, and ventral curvature are considered poor prognostic factors for good
functional outcomes after grafting surgery [1095]. Although the risk for penile shortening appears to be less
than that compared to the Nesbit, Yachia or plication procedures, it is still an issue and patients must be
informed accordingly [1094]. Higher rates (3-52%) of penile hypo-aesthesia have also been described after
these operations, as damage of the neurovascular bundle with dorsal curves (in the majority) is inevitable. A
recent prospective study showed that 21% of patients had some degree of sensation loss at 1 week, 21% at
1 month, 8% at 6 months, and 3% at 1 year [1143]. The use of geometric principles introduced by Egydio may
help to determine the exact site of the incision, and the shape and size of the defect to be grafted [1144].
Grafts for PD surgery can be classified into four types (Table 31) [994]:
• Autografts: taken from the individual himself, they include the dermis, vein, temporalis fascia, fascia lata,
tunica vaginalis, tunica albuginea and buccal mucosa.
• Allografts: also of human origin but from a deceased donor, including the pericardium, fascia lata and
dura mater.
• Xenografts: extracted from different animal species and tissues, including bovine pericardium, porcine
small intestinal submucosa, bovine and porcine dermis, and TachoSil (matrix of equine collagen).
®
®
• Synthetic grafts: these include Dacron and Gore-Tex .
®
SEXUAL AND REPRODUCTIVE HEALTH - MARCH 2021 101