Page 34 - Remedial Andrology
P. 34
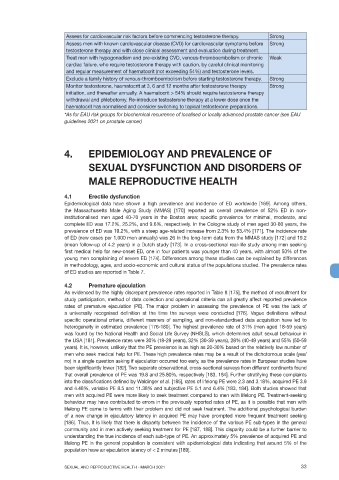
Assess for cardiovascular risk factors before commencing testosterone therapy. Strong
Assess men with known cardiovascular disease (CVD) for cardiovascular symptoms before Strong
testosterone therapy and with close clinical assessment and evaluation during treatment.
Treat men with hypogonadism and pre-existing CVD, venous-thromboembolism or chronic Weak
cardiac failure, who require testosterone therapy with caution, by careful clinical monitoring
and regular measurement of haematocrit (not exceeding 54%) and testosterone levels.
Exclude a family history of venous-thromboembolism before starting testosterone therapy. Strong
Monitor testosterone, haematocrit at 3, 6 and 12 months after testosterone therapy Strong
initiation, and thereafter annually. A haematocrit > 54% should require testosterone therapy
withdrawal and phlebotomy. Re-introduce testosterone therapy at a lower dose once the
haematocrit has normalised and consider switching to topical testosterone preparations.
*As for EAU risk groups for biochemical recurrence of localised or locally advanced prostate cancer (see EAU
guidelines 2021 on prostate cancer)
4. EPIDEMIOLOGY AND PREVALENCE OF
SEXUAL DYSFUNCTION AND DISORDERS OF
MALE REPRODUCTIVE HEALTH
4.1 Erectile dysfunction
Epidemiological data have shown a high prevalence and incidence of ED worldwide [169]. Among others,
the Massachusetts Male Aging Study (MMAS) [170] reported an overall prevalence of 52% ED in non-
institutionalised men aged 40-70 years in the Boston area; specific prevalence for minimal, moderate, and
complete ED was 17.2%, 25.2%, and 9.6%, respectively. In the Cologne study of men aged 30-80 years, the
prevalence of ED was 19.2%, with a steep age-related increase from 2.3% to 53.4% [171]. The incidence rate
of ED (new cases per 1,000 men annually) was 26 in the long-term data from the MMAS study [172] and 19.2
(mean follow-up of 4.2 years) in a Dutch study [173]. In a cross-sectional real-life study among men seeking
first medical help for new-onset ED, one in four patients was younger than 40 years, with almost 50% of the
young men complaining of severe ED [174]. Differences among these studies can be explained by differences
in methodology, ages, and socio-economic and cultural status of the populations studied. The prevalence rates
of ED studies are reported in Table 7.
4.2 Premature ejaculation
As evidenced by the highly discrepant prevalence rates reported in Table 8 [175], the method of recruitment for
study participation, method of data collection and operational criteria can all greatly affect reported prevalence
rates of premature ejaculation (PE). The major problem in assessing the prevalence of PE was the lack of
a universally recognised definition at the time the surveys were conducted [176]. Vague definitions without
specific operational criteria, different manners of sampling, and non-standardised data acquisition have led to
heterogeneity in estimated prevalence [176-180]. The highest prevalence rate of 31% (men aged 18-59 years)
was found by the National Health and Social Life Survey (NHSLS), which determines adult sexual behaviour in
the USA [181]. Prevalence rates were 30% (18-29 years), 32% (30-39 years), 28% (40-49 years) and 55% (50-59
years). It is, however, unlikely that the PE prevalence is as high as 20-30% based on the relatively low number of
men who seek medical help for PE. These high prevalence rates may be a result of the dichotomous scale (yes/
no) in a single question asking if ejaculation occurred too early, as the prevalence rates in European studies have
been significantly lower [182]. Two separate observational, cross-sectional surveys from different continents found
that overall prevalence of PE was 19.8 and 25.80%, respectively [183, 184]. Further stratifying these complaints
into the classifications defined by Waldinger et al. [185], rates of lifelong PE were 2.3 and 3.18%, acquired PE 3.9
and 4.48%, variable PE 8.5 and 11.38% and subjective PE 5.1 and 6.4% [183, 184]. Both studies showed that
men with acquired PE were more likely to seek treatment compared to men with lifelong PE. Treatment-seeking
behaviour may have contributed to errors in the previously reported rates of PE, as it is possible that men with
lifelong PE came to terms with their problem and did not seek treatment. The additional psychological burden
of a new change in ejaculatory latency in acquired PE may have prompted more frequent treatment seeking
[186]. Thus, it is likely that there is disparity between the incidence of the various PE sub-types in the general
community and in men actively seeking treatment for PE [187, 188]. This disparity could be a further barrier to
understanding the true incidence of each sub-type of PE. An approximately 5% prevalence of acquired PE and
lifelong PE in the general population is consistent with epidemiological data indicating that around 5% of the
population have an ejaculation latency of < 2 minutes [189].
SEXUAL AND REPRODUCTIVE HEALTH - MARCH 2021 33