Page 157 - Remedial Andrology
P. 157
subsequent ICSI procedures [1847]. Patency rates range between 65% and 85% and cumulative pregnancy
rates between 21% and 44% [1840, 1866]. Recanalisation success rates may be adversely affected by pre-
operative and intra-operative findings. Robot-assisted EV has similar success rates and larger studies are
needed [1720].
10.6.1.3.3 Vas deferens obstruction after vasectomy
Vas deferens obstruction after vasectomy requires microsurgical vasectomy reversal. The mean post-
procedural patency and pregnancy rates weighted by sample size were 90-97% and 52-73%, respectively
[1840, 1866]. The average time to patency is 1.7-4.3 months and late failures are uncommon (0-12%) [1865].
Robot-assisted vasovasostomy has similar success rates, and larger studies, including cost-benefit analysis,
are needed to establish its benefits over standard microsurgical procedures [1720].
The absence of spermatozoa in the intra-operative vas deferens fluid suggests the presence of
a secondary epididymal obstruction, especially if the seminal fluid of the proximal vas deferens has a thick
“toothpaste” appearance; in this case microsurgical EV may be indicated [1867-1869]. Simultaneous sperm
retrieval may be performed for future cryopreservation and use for ICSI; likewise, patients should be counselled
appropriately.
10.6.1.3.4 Vas deferens obstruction at the inguinal level
It is usually impossible to correct large bilateral vas deferens defects, resulting from involuntary excision of
the vasa deferentia during hernia surgery in early childhood or previous orchidopexy. In these cases, TESE/
MESA/PESA or proximal vas deferens sperm aspiration [1870] can be used for cryopreservation for future ICSI.
Prostate cancer patients who express an interest in future fertility should be counselled for cryopreservation
[1871, 1872].
10.6.1.3.5 Ejaculatory duct obstruction
The treatment of ejaculatory duct obstruction (EDO) depends on its aetiology. Transurethral resection of the
ejaculatory ducts (TURED) can be used in post-inflammatory obstruction and cystic obstruction [1843, 1847].
Resection may remove part of the verumontanum. In cases of obstruction due to a midline intraprostatic cyst,
incision, unroofing or aspiration of the cyst is required [1843, 1847].
Intra-operative TRUS makes this procedure safer. If distal seminal tract evaluation is carried out at the time
of the procedure, installation of methylene blue dye into the seminal vesicles (chromotubation) can help to
confirm intra-operative opening of the ducts. Pregnancy rates after TURED are 20-25% [1664, 1843, 1873].
Complications following TURED include epididymitis, UTI, gross haematuria, haematospermia, azoospermia
(in cases with partial distal ejaculatory duct obstruction) and urine reflux into the ejaculatory ducts and seminal
vesicles [1843].
Alternative therapies for EDO include, seminal vesiculoscopy to remove debris or calculi and balloon dilation
and laser incision for calcification on TRUS [1874]. The alternatives to TURED are MESA, PESA, TESE,
proximal vas deferens sperm aspiration and seminal vesicle-ultrasonically guided aspiration.
10.6.1.4 Summary of evidence and recommendations for obstructive azoospermia
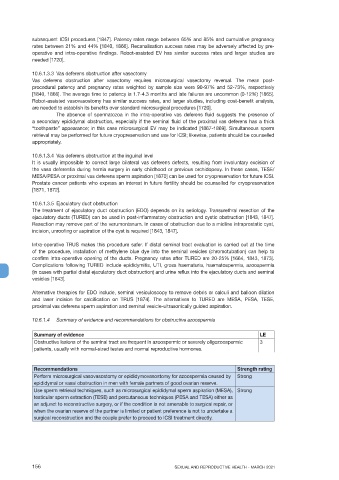
Summary of evidence LE
Obstructive lesions of the seminal tract are frequent in azoospermic or severely oligozoospermic 3
patients, usually with normal-sized testes and normal reproductive hormones.
Recommendations Strength rating
Perform microsurgical vasovasostomy or epididymovasostomy for azoospermia caused by Strong
epididymal or vasal obstruction in men with female partners of good ovarian reserve.
Use sperm retrieval techniques, such as microsurgical epididymal sperm aspiration (MESA), Strong
testicular sperm extraction (TESE) and percutaneous techniques (PESA and TESA) either as
an adjunct to reconstructive surgery, or if the condition is not amenable to surgical repair, or
when the ovarian reserve of the partner is limited or patient preference is not to undertake a
surgical reconstruction and the couple prefer to proceed to ICSI treatment directly.
156 SEXUAL AND REPRODUCTIVE HEALTH - MARCH 2021