Page 155 - Remedial Andrology
P. 155
10.6.1.1 Classification of obstructive azoospermia
10.6.1.1.1 Intratesticular obstruction
Intratesticular obstruction occurs in 15% of men with OA [1832]. Congenital forms are less common than
acquired forms (post-inflammatory or post-traumatic) (Table 42).
10.6.1.1.2 Epididymal obstruction
Epididymal obstruction is the most common cause of OA, affecting 30-67% of azoospermic men [1832-1835].
Congenital epididymal obstruction usually manifests as CBAVD, which is associated with at least one mutation
of the CF gene in 82% of cases [1835]. Other congenital forms of epididymal obstruction include chronic sinu-
pulmonary infections (Young’s syndrome) [1836]. Acquired forms secondary to acute (e.g., gonococcal) and
subclinical (e.g., Chlamydial) epididymitis are most commonly due to infections [1837, 1838]. Other causes may
be trauma or surgical intervention [1839, 1840] (Table 42).
10.6.1.1.3 Vas deferens obstruction
Vas deferens obstruction is the most common cause of acquired obstruction following vasectomy [1837]
(Table 42). Approximately 2-6 % of these men request vasectomy reversal (see 2019 EAU Guidelines on Male
Infertility). Vasal obstruction may also occur after hernia repair [1841, 1842]. The most common congenital
vasal obstruction is CBAVD, often accompanied by CF. Unilateral agenesis or a partial defect is associated with
contralateral seminal duct anomalies or renal agenesis in 80% and 26% of cases, respectively [1524].
10.6.1.1.4 Ejaculatory duct obstruction
Ejaculatory duct obstruction is found in 1-5% of cases of OA and is classified as cystic or post-inflammatory
or calculi of one or both ejaculatory ducts [1664, 1843] (Table 42). Cystic obstructions are usually congenital
(i.e., Mullerian duct cyst or urogenital sinus/ejaculatory duct cysts) and are typically midline. In urogenital
sinus abnormalities, one or both ejaculatory ducts empty into the cyst [1844], while in Mullerian duct
anomalies, the ejaculatory ducts are laterally displaced and compressed by the cyst [1845]. Paramedian or
lateral intraprostatic cysts are rare [1846]. Post-inflammatory obstructions of the ejaculatory duct are usually
secondary to urethra-prostatitis [1847]. Congenital or acquired complete obstructions of the ejaculatory ducts
are commonly associated with low seminal volume, decreased or absent seminal fructose, and acidic pH. The
seminal vesicles (anterior-posterior diameter > 15 mm) and ejaculatory duct (> 2.3 mm in width) are usually
dilated [1843, 1847-1849].
10.6.1.1.4.1 Functional obstruction of the distal seminal ducts
Functional obstruction of the distal seminal ducts might be attributed to local neurogenic dysfunction [1850].
This abnormality is often associated with urodynamic dysfunction. Impaired sperm transport can be observed
as idiopathic or due to spinal cord injury, multiple sclerosis, retroperitoneal lymph node dissection, pelvic
surgery, SSRIs, α-blockers and typical antipsychotic medications [1851].
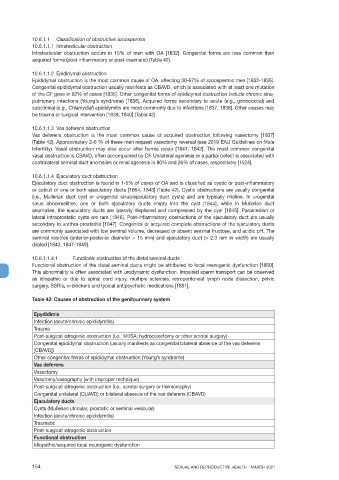
Table 42: Causes of obstruction of the genitourinary system
Epydidimis
Infection (acute/chronic epididymitis)
Trauma
Post-surgical iatrogenic obstruction (i.e., MESA; hydrocelectomy or other scrotal surgery)
Congenital epididymal obstruction (usually manifests as congenital bilateral absence of the vas deferens
[CBAVD])
Other congenital forms of epididymal obstruction (Young’s syndrome)
Vas deferens
Vasectomy
Vasotomy/vasography (with improper technique)
Post-surgical iatrogenic obstruction (i.e., scrotal surgery or herniorraphy)
Congenital unilateral (CUAVD) or bilateral absence of the vas deferens (CBAVD)
Ejaculatory ducts
Cysts (Mullerian utricular, prostatic or seminal vesicular)
Infection (acute/chronic epididymitis)
Traumatic
Post-surgical iatrogenic obstruction
Functional obstruction
Idiopathic/acquired local neurogenic dysfunction
154 SEXUAL AND REPRODUCTIVE HEALTH - MARCH 2021