Page 148 - Remedial Andrology
P. 148
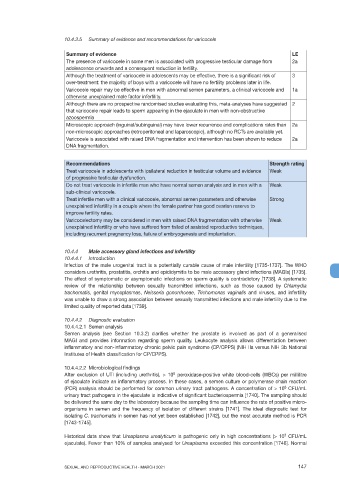
10.4.3.5 Summary of evidence and recommendations for varicocele
Summary of evidence LE
The presence of varicocele in some men is associated with progressive testicular damage from 2a
adolescence onwards and a consequent reduction in fertility.
Although the treatment of varicocele in adolescents may be effective, there is a significant risk of 3
over-treatment: the majority of boys with a varicocele will have no fertility problems later in life.
Varicocele repair may be effective in men with abnormal semen parameters, a clinical varicocele and 1a
otherwise unexplained male factor infertility.
Although there are no prospective randomised studies evaluating this, meta-analyses have suggested 2
that varicocele repair leads to sperm appearing in the ejaculate in men with non-obstructive
azoospermia
Microscopic approach (inguinal/subinguinal) may have lower recurrence and complications rates than 2a
non-microscopic approaches (retroperitoneal and laparoscopic), although no RCTs are available yet.
Varicocele is associated with raised DNA fragmentation and intervention has been shown to reduce 2a
DNA fragmentation.
Recommendations Strength rating
Treat varicocele in adolescents with ipsilateral reduction in testicular volume and evidence Weak
of progressive testicular dysfunction.
Do not treat varicocele in infertile men who have normal semen analysis and in men with a Weak
sub-clinical varicocele.
Treat infertile men with a clinical varicocele, abnormal semen parameters and otherwise Strong
unexplained infertility in a couple where the female partner has good ovarian reserve to
improve fertility rates.
Varicocelectomy may be considered in men with raised DNA fragmentation with otherwise Weak
unexplained infertility or who have suffered from failed of assisted reproductive techniques,
including recurrent pregnancy loss, failure of embryogenesis and implantation.
10.4.4 Male accessory gland infections and infertility
10.4.4.1 Introduction
Infection of the male urogenital tract is a potentially curable cause of male infertility [1735-1737]. The WHO
considers urethritis, prostatitis, orchitis and epididymitis to be male accessory gland infections (MAGIs) [1735].
The effect of symptomatic or asymptomatic infections on sperm quality is contradictory [1738]. A systematic
review of the relationship between sexually transmitted infections, such as those caused by Chlamydia
trachomatis, genital mycoplasmas, Neisseria gonorrhoeae, Trichomonas vaginalis and viruses, and infertility
was unable to draw a strong association between sexually transmitted infections and male infertility due to the
limited quality of reported data [1739].
10.4.4.2 Diagnostic evaluation
10.4.4.2.1 Semen analysis
Semen analysis (see Section 10.3.2) clarifies whether the prostate is involved as part of a generalised
MAGI and provides information regarding sperm quality. Leukocyte analysis allows differentiation between
inflammatory and non-inflammatory chronic pelvic pain syndrome (CP/CPPS) (NIH IIa versus NIH 3b National
Institutes of Health classification for CP/CPPS).
10.4.4.2.2 Microbiological findings
6
After exclusion of UTI (including urethritis), > 10 peroxidase-positive white blood-cells (WBCs) per millilitre
of ejaculate indicate an inflammatory process. In these cases, a semen culture or polymerase chain reaction
(PCR) analysis should be performed for common urinary tract pathogens. A concentration of > 10 CFU/mL
3
urinary tract pathogens in the ejaculate is indicative of significant bacteriospermia [1740]. The sampling should
be delivered the same day to the laboratory because the sampling time can influence the rate of positive micro-
organisms in semen and the frequency of isolation of different strains [1741]. The ideal diagnostic test for
isolating C. trachomatis in semen has not yet been established [1742], but the most accurate method is PCR
[1743-1745].
3
Historical data show that Ureaplasma urealyticum is pathogenic only in high concentrations (> 10 CFU/mL
ejaculate). Fewer than 10% of samples analysed for Ureaplasma exceeded this concentration [1746]. Normal
SEXUAL AND REPRODUCTIVE HEALTH - MARCH 2021 147