Page 139 - Remedial Andrology
P. 139
related to the obstruction of the ejaculatory ducts, such as ejaculatory duct cysts, seminal vesicular dilatation or
hypoplasia/atrophy, although retrograde ejaculation should be excluded as a differential diagnosis [1458, 1619].
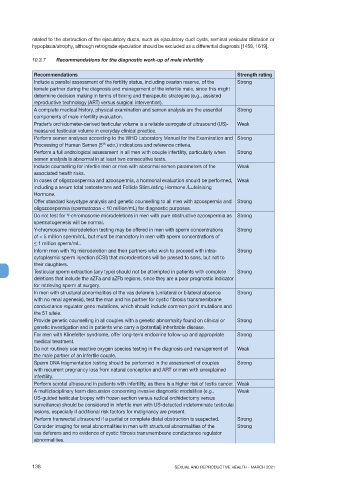
10.3.7 Recommendations for the diagnostic work-up of male infertility
Recommendations Strength rating
Include a parallel assessment of the fertility status, including ovarian reserve, of the Strong
female partner during the diagnosis and management of the infertile male, since this might
determine decision making in terms of timing and therapeutic strategies (e.g., assisted
reproductive technology (ART) versus surgical intervention).
A complete medical history, physical examination and semen analysis are the essential Strong
components of male infertility evaluation.
Prader’s orchidometer-derived testicular volume is a reliable surrogate of ultrasound (US)- Weak
measured testicular volume in everyday clinical practice.
Perform semen analyses according to the WHO Laboratory Manual for the Examination and Strong
th
Processing of Human Semen (5 edn.) indications and reference criteria.
Perform a full andrological assessment in all men with couple infertility, particularly when Strong
semen analysis is abnormal in at least two consecutive tests.
Include counselling for infertile men or men with abnormal semen parameters of the Weak
associated health risks.
In cases of oligozoospermia and azoospermia, a hormonal evaluation should be performed, Weak
including a serum total testosterone and Follicle Stimulating Hormone /Luteinising
Hormone.
Offer standard karyotype analysis and genetic counselling to all men with azoospermia and Strong
oligozoospermia (spermatozoa < 10 million/mL) for diagnostic purposes.
Do not test for Y-chromosome microdeletions in men with pure obstructive azoospermia as Strong
spermatogenesis will be normal.
Y-chromosome microdeletion testing may be offered in men with sperm concentrations Strong
of < 5 million sperm/mL, but must be mandatory in men with sperm concentrations of
< 1 million sperm/mL.
Inform men with Yq microdeletion and their partners who wish to proceed with intra- Strong
cytoplasmic sperm injection (ICSI) that microdeletions will be passed to sons, but not to
their daughters.
Testicular sperm extraction (any type) should not be attempted in patients with complete Strong
deletions that include the aZFa and aZFb regions, since they are a poor prognostic indicator
for retrieving sperm at surgery.
In men with structural abnormalities of the vas deferens (unilateral or bilateral absence Strong
with no renal agenesis), test the man and his partner for cystic fibrosis transmembrane
conductance regulator gene mutations, which should include common point mutations and
the 5T allele.
Provide genetic counselling in all couples with a genetic abnormality found on clinical or Strong
genetic investigation and in patients who carry a (potential) inheritable disease.
For men with Klinefelter syndrome, offer long-term endocrine follow-up and appropriate Strong
medical treatment.
Do not routinely use reactive oxygen species testing in the diagnosis and management of Weak
the male partner of an infertile couple.
Sperm DNA fragmentation testing should be performed in the assessment of couples Strong
with recurrent pregnancy loss from natural conception and ART or men with unexplained
infertility.
Perform scrotal ultrasound in patients with infertility, as there is a higher risk of testis cancer. Weak
A multidisciplinary team discussion concerning invasive diagnostic modalities (e.g., Weak
US-guided testicular biopsy with frozen section versus radical orchidectomy versus
surveillance) should be considered in infertile men with US-detected indeterminate testicular
lesions, especially if additional risk factors for malignancy are present.
Perform transrectal ultrasound if a partial or complete distal obstruction is suspected. Strong
Consider imaging for renal abnormalities in men with structural abnormalities of the Strong
vas deferens and no evidence of cystic fibrosis transmembrane conductance regulator
abnormalities.
138 SEXUAL AND REPRODUCTIVE HEALTH - MARCH 2021